A Multi-Faceted Approach to Tuberculosis Active Case Finding among Remote Riverine Communities in Southern Nigeria
Abstract
:1. Introduction
2. Methods
2.1. Intervention
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Intervention Notification Data
3.2. Observations from the Field
3.2.1. Impact and Reception of the Intervention
3.2.2. Perception of the Three Different Approaches
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Global Tuberculosis Report 2020 [Internet]. Geneva. Available online: https://www.who.int/publications/i/item/9789240013131 (accessed on 27 November 2020).
- Floyd, K.; Glaziou, P.; Houben, R.M.G.J.; Sumner, T.; White, R.G.; Raviglione, M. Global tuberculosis targets and milestones set for 2016-2035: Definition and rationale. Int. J. Tuberc. Lung. Dis. 2018, 22, 723–730. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Joint Initiative “Find. Treat. All. #ENDTB” [Internet]. Available online: https://www.who.int/tb/joint-initiative/en/ (accessed on 5 February 2021).
- Ogbudebe, C.L.; Chukwu, J.N.; Nwafor, C.C.; Meka, A.O.; Ekeke, N.; Madichie, N.O.; Anyim, M.C.; Osakwe, C.; Onyeonoro, U.; Ukwaja, K.N.; et al. Reaching the underserved: Active tuberculosis case finding in urban slums in southeastern Nigeria. Int. J. Mycobacteriol. 2015, 4, 18–24. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adepoju, P. Nigeria’s widening tuberculosis gap. Lancet Infect. Dis. 2020, 20, 29. [Google Scholar] [CrossRef]
- Ologbon, O.A.C.; Idowu, A.O.; Salmonu, K.K.; Oluwatayo, I.B. Incidence of multidimensional poverty among riverine households in Southwestern Nigeria. J. Agric. Sci. 2014, 6. [Google Scholar] [CrossRef] [Green Version]
- Afe Abayomi, J.; Edet-Utan, O.; Fadero, T.; Akinmurele, T. Heath-seeking behavior of riverine residents of Arogbo-Ijaw island in ese-odo local government area of ondo state, Southwest Nigeria. S. Am. J. Acad. Res. 2015, 2. Available online: https://www.researchgate.net/publication/271515545_HEATH-SEEKING_BEHAVIOR_OF_RIVERINE_RESIDENTS_OF_AROGBO-IJAW_ISLAND_IN_ESE-ODO_LOCAL_GOVERNMENT_AREA_OF_ONDO_STATESOUTHWEST_NIGERIA (accessed on 29 July 2021).
- Ofili, M.I.; Ncama, B.P.; Sartorius, B. Hypertension in rural communities in Delta State, Nigeria: Prevalence, risk factors and barriers to health care. Afr. J. Prim. Health Care Fam. Med. 2015, 7, 7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ukwaja, K.N.; Alobu, I.; Nweke, C.O.; Onyenwe, E.C. Healthcare-seeking behavior, treatment delays and its determinants among pulmonary tuberculosis patients in rural Nigeria: A cross-sectional study. BMC Health Serv. Res. 2013, 13, 25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bamgboye, M.; Ezedinachi, E.; Bassey, I.; Iwara, A. Raising awareness about Tuberculosis among women living in rural communities on the Atlantic coastline of Nigeria. Transl. Biomed. 2016, 7, 3. [Google Scholar]
- Blok, L.; Creswell, J.; Stevens, R.; Brouwer, M.; Ramis, O.; Weil, O.; Klatser, P.; Sahu, S.; Bakker, M.I. A pragmatic approach to measuring, monitoring and evaluating interventions for improved tuberculosis case detection. Int. Health 2014, 6, 181–188. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vyas, A.; Creswell, J.; Codlin, A.J.; Stevens, R.; Rao, V.G.; Kumar, B.; Khaparde, S.; Sahu, S. Community-based active case-finding to reach the most vulnerable: Tuberculosis in tribal areas of India. Int. J. Tuberc. Lung Dis. 2019, 23, 750–755. [Google Scholar] [CrossRef] [PubMed]
- Abdullahi, S.A.; Smelyanskaya, M.; John, S.; Adamu, H.I.; Ubochioma, E.; Kennedy, I.; Abubakar, F.A.; Ago, H.A.; Stevens, R.; Creswell, J. Providing TB and HIV outreach services to internally displaced populations in Northeast Nigeria: Results of a controlled intervention study. PLoS Med. 2020, 17, e1003218. [Google Scholar] [CrossRef]
- Chikovore, J.; Pai, M.; Horton, K.C.; Daftary, A.; Kumwenda, M.K.; Hart, G.; Corbett, E.L. Missing men with tuberculosis: The need to address structural influences and implement targeted and multidimensional interventions. BMJ Glob. Health 2020, 5, e002255. [Google Scholar] [CrossRef] [PubMed]
- Oshi, D.C.; Chukwu, J.N.; Nwafor, C.C.; Meka, A.O.; Madichie, N.O.; Ogbudebe, C.L.; Onyeonoro, U.U.; Ikebudu, J.N.; Ekeke, N.; Anyim, M.C.; et al. Does intensified case finding increase tuberculosis case notification among children in resource-poor settings? A report from Nigeria. Int. J. Mycobacteriol. 2016, 5, 44–50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Roadmap for Childhood Tuberculosis: Towards Zero Deaths [Internet]. Geneva. 2013. Available online: http://apps.who.int/iris/bitstream/handle/10665/89506/9789241506137_eng.pdf;jsessionid=9719130E0F339BCCD67DEA533A706CEC?sequence=1 (accessed on 29 July 2021).
- Fox, G.J.; Barry, S.E.; Britton, W.J.; Marks, G.B. Contact investigation for tuberculosis: A systematic review and meta-analysis. Eur. Respir. J. 2013, 41, 140–156. [Google Scholar] [CrossRef] [PubMed]
- Oshi, D.; Omeje, J.; Oshi, S.; Alobu, I.; Chukwu, N.; Nwokocha, C.; Emelumadu, O.; Ogbudebe, C.; Meka, A.; Ukwaja, K.N. An evaluation of innovative community-based approaches and systematic tuberculosis screening to improve tuberculosis case detection in Ebonyi State, Nigeria. Int. J. Mycobacteriol. 2017, 6, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Mehboob, N.; Rahman-Shepherd, A.; Naureen, F.; Rashid, A.; Buzdar, N.; Ishaq, M. What can motivate lady health workers in Pakistan to engage more actively in tuberculosis case-finding? BMC Public Health 2019, 19, 999. [Google Scholar] [CrossRef] [PubMed]
- Pande, T.; Vasquez, N.A.; Cazabon, D.; Creswell, J.; Brouwer, M.; Ramis, O.; Stevens, R.H.; Ananthakrishnan, R.; Qayyum, S.; Alphonsus, C.; et al. Finding the missing millions: Lessons from 10 active case finding interventions in high tuberculosis burden countries. BMJ Glob. Health 2020, 5, e003835. [Google Scholar] [CrossRef] [PubMed]
- Cattamanchi, A.; Berger, C.A.; Shete, P.B.; Turyahabwe, S.; Joloba, M.; Moore, D.A.; Davis, J.L.; Katamba, A. Implementation science to improve the quality of tuberculosis diagnostic services in Uganda. J. Clin. Tuberc. Other Mycobact. Dis. 2019, 18, 100136. [Google Scholar] [CrossRef] [PubMed]

| Total N (%) | Male N (%) | Female N (%) | |
|---|---|---|---|
| Number of people screened | 509,768 | 241,745 | 268,023 |
| Number of individuals with presumptive TB (% among screened) | 12,247 (2.4) | 5443 (2.3) | 6804 (2.5) |
| Number tested for TB (% among individuals with presumptive TB) | 11,824 (96.5) | 5236 (96.2) | 6588 (96.8) |
| Number of people with Bac+ 1 TB (% among tested) | 808 (6.8) | 436 (8.3) | 372 (5.6) |
| Number of individuals diagnosed with all forms 2 TB (% among individuals with presumptive TB) | 1015 (8.3) | 539 (9.9) | 476 (7.0) |
| Number of individuals with Bac+ TB started on treatment (% among Bac+ 1 TB) | 794 (98.2) | 432 (99.1) | 362 (97.3) |
| Number of individuals with all forms TB started on treatment (% all forms TB) | 1001 (98.6) | 532 (98.7) | 469 (98.5) |
| Number of individuals with Bac+ TB who completed treatment (% started treatment) | 794 (100.0) | 432 (100.0) | 362 (100.0) |
| Number of individuals with all forms TB who completed treatment (% started treatment) | 1001 (100.0) | 532 (100.0) | 469 (100.0) |
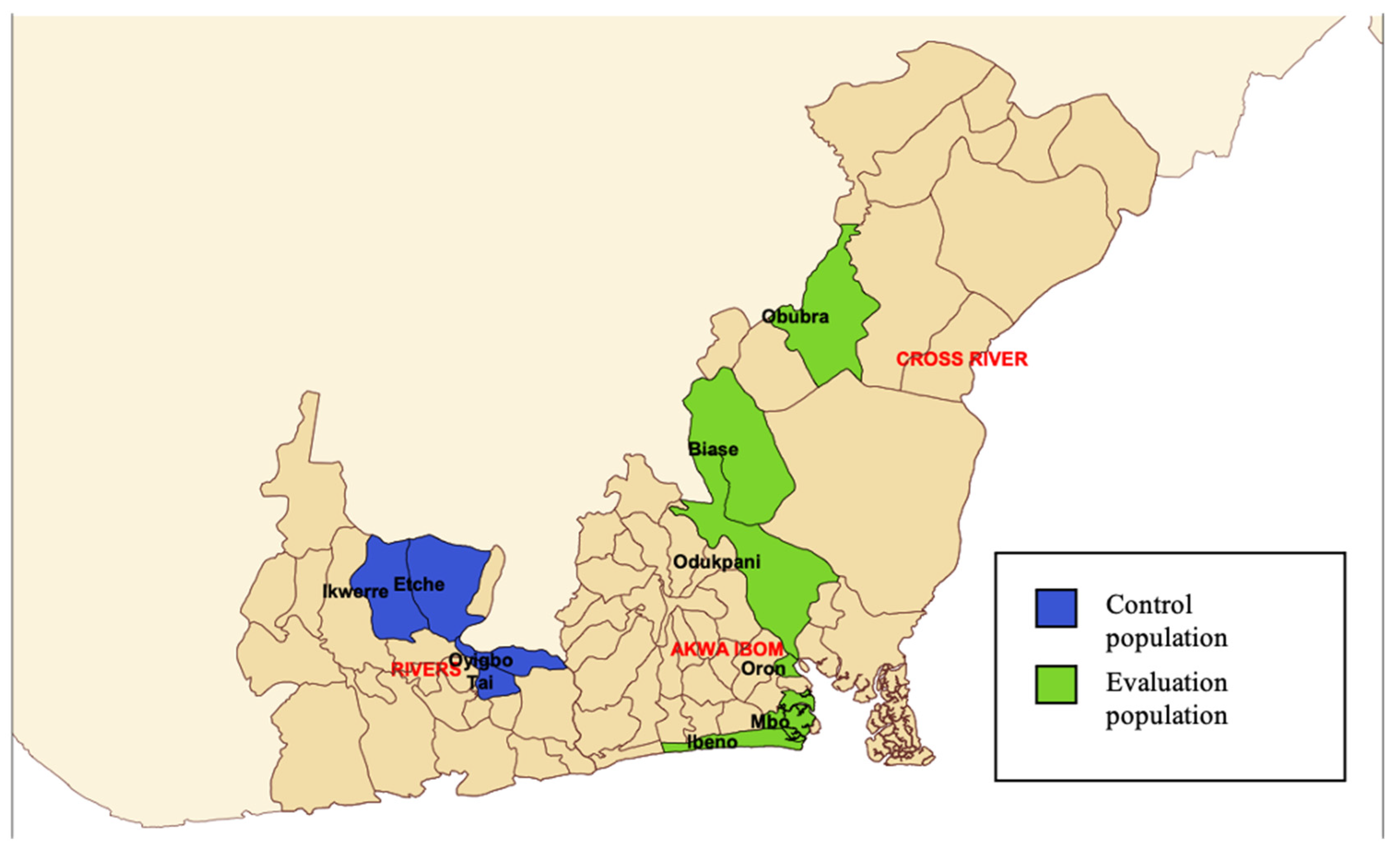
| Evaluation Population | Control Population | |||
|---|---|---|---|---|
| Bac+ | All Forms | Bac+ | All Forms | |
| Baseline notification data (2017–2018) | 518 | 591 | 226 | 204 |
| Notifications during implementation | 921 | 1258 | 365 | 410 |
| Unadjusted additional notifications | 403 | 667 | 139 | 206 |
| % change from baseline | 77.8% | 112.9% | 61.5% | 101.0% |
| Expected notifications (without intervention) * | 534 | 528 | 225 | 275 |
| Adjusted additional notifications | 387 | 730 | 140 | 135 |
| % change from expected notifications | 72.5% | 138.3% | 62.2% | 49.1% |
| 0–4 Years | 5–14 Years | Total | |
|---|---|---|---|
| Baseline childhood TB notifications (2017–2018) | 5 | 11 | 16 |
| Notifications during implementation | 27 | 94 | 121 |
| Additional notifications | 22 | 83 | 105 |
| % change from baseline | 440% | 755% | 656% |
| Community Outreach | H2H/T2T 1 Screening | Contact Investigation | |
|---|---|---|---|
| Number of people screened | 209,177 | 269,069 | 11,700 |
| Number of individuals with presumptive TB (% among screened) | 4536 (2.2) | 5786 (2.2) | 1350 (11.5) |
| Number tested for TB (% among individuals with presumptive TB) | 4405 (97.1) | 5509 (95.2) | 1350 (100.0) |
| Number of people with Bac+ TB (% among tested) | 283 (6.4) | 386 (7.0) | 95 (7.0) |
| Number of people diagnosed with all forms TB (% among individuals with presumptive TB) | 385 (8.5) | 461 (8.0) | 105 (7.8) |
| Number of individuals with Bac+ TB started on treatment (% among Bac+ TB) | 278 (98.2) | 377 (97.7) | 95 (100.0) |
| Number of individuals with all forms TB started on treatment (% all forms TB) | 385 (100.0) | 452 (98.0) | 105 (100.0) |
| Number of individuals with Bac+ TB who completed treatment (% started treatment) | 278 (100.0) | 377 (100.0) | 95 (100.0) |
| Number of individuals with all forms TB who completed treatment (% started treatment) | 385 (100.0) | 452 (100.0) | 105 (100.0) |
| Number needed to screen to diagnose one TB case (all forms) | 543 | 583 | 111 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Eyo, A.S.; Obot, V.O.; Onyedinachi, O.; Aguilera Vasquez, N.; Bigio, J.; Sanaie, A.; Beulah, F.; Ette, U.; Uju, D.; Rahman, M.T. A Multi-Faceted Approach to Tuberculosis Active Case Finding among Remote Riverine Communities in Southern Nigeria. Int. J. Environ. Res. Public Health 2021, 18, 9424. https://doi.org/10.3390/ijerph18189424
Eyo AS, Obot VO, Onyedinachi O, Aguilera Vasquez N, Bigio J, Sanaie A, Beulah F, Ette U, Uju D, Rahman MT. A Multi-Faceted Approach to Tuberculosis Active Case Finding among Remote Riverine Communities in Southern Nigeria. International Journal of Environmental Research and Public Health. 2021; 18(18):9424. https://doi.org/10.3390/ijerph18189424
Chicago/Turabian StyleEyo, Andy Samuel, Valerie Okon Obot, Okezie Onyedinachi, Nathaly Aguilera Vasquez, Jacob Bigio, Ataulhaq Sanaie, Favour Beulah, Uduak Ette, Dennis Uju, and Md. Toufiq Rahman. 2021. "A Multi-Faceted Approach to Tuberculosis Active Case Finding among Remote Riverine Communities in Southern Nigeria" International Journal of Environmental Research and Public Health 18, no. 18: 9424. https://doi.org/10.3390/ijerph18189424







